|
Trauma Series - Part 4 of 7
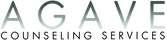
Research on trauma plays a vital role in unraveling the complex interplay between traumatic experiences and mental health outcomes, shedding light on effective prevention strategies, evidence-based treatments, and policy initiatives aimed at supporting and empowering survivors of trauma. The following studies have had profound effects on the lanscape and scope of trauma treatment and should be accounted for within any historical perspective of trauma as a whole.
NVVRS - 1988 The National Vietnam Veterans Readjustment Study (NVVRS) is a comprehensive examination of post-traumatic stress disorder (PTSD) and psychological difficulties among Vietnam veterans. The study provides valuable insights into the challenges faced by these veterans as they transitioned to civilian life. Key findings from the study include the higher prevalence of PTSD among Vietnam theater veterans compared to their era counterparts and civilians, with rates of 15.2% for males and 8.5% for females. Additionally, the study highlights the lasting nature of PTSD, with one-third of male theater veterans and over one-fourth of female theater veterans having experienced the disorder at some point in their lives. The research underscores the link between PTSD and other readjustment difficulties and emphasizes the impact on veterans' families. The study emphasizes the need for ongoing support and care for Vietnam veterans affected by these psychological issues. HTQ – 1992 The Harvard Trauma Questionnaire (HTQ) is a checklist that was developed by the Harvard Program in Refugee Trauma (HPRT) to assess trauma events and associated emotional symptoms. It consists of six versions tailored to different populations, including Southeast Asian refugees, survivors of the Kobe earthquake, Croatian veterans, and Bosnian civilians. The questionnaire covers a range of traumatic experiences and includes sections on traumatic events, subjective descriptions of the most traumatic events, head injuries, and trauma symptoms. While earlier versions offered multiple response options, later versions simplified the responses to "Yes" or "No" for each question. The HTQ includes items derived from the DSM-IV criteria for post-traumatic stress disorder (PTSD) and additional culture-specific questions. It is important to note that the HTQ is intended for administration by healthcare professionals and should not be used as a self-report tool. The involvement of mental health professionals is crucial in the proper use and interpretation of screening instruments. NCS – 1995 The National Comorbidity Survey (NCS) is a series of surveys conducted in the United States to assess the prevalence and comorbidity of mental disorders among adults, including post-traumatic stress disorder (PTSD). The study aims to understand the prevalence, risk factors, and patterns of comorbidity associated with PTSD, as well as its impact on functioning and quality of life. The NCS findings contribute to our understanding of PTSD's epidemiology and public health impact, informing interventions and support systems for affected individuals. The study highlights that PTSD is a prevalent and persistent disorder influenced by factors such as gender and marital status, and future research should consider assessing PTSD for all lifetime traumas to gain a comprehensive understanding. ACE Study – 1998 The ACEs study is a groundbreaking research effort that examines the impact of adverse childhood experiences (ACEs) on long-term health and well-being. It demonstrates a strong association between childhood trauma and the development of various physical, mental, and social health problems later in life. The study highlights the cumulative nature of ACEs and their profound influence on individuals' overall health outcomes. The findings underscore the importance of early intervention and prevention strategies to mitigate the long-term consequences of childhood adversity. NISVS – 2011 The National Intimate Partner and Sexual Violence Survey (NISVS) conducted in 2011 is a comprehensive study that examines the prevalence, impact, and consequences of intimate partner violence, sexual violence, and stalking in the United States. The survey provides valuable insights into the scope and nature of these forms of violence, highlighting their high prevalence and the significant physical and mental health consequences experienced by survivors. The NISVS data contribute to the understanding of these public health issues, informing policies, prevention efforts, and support services for victims of intimate partner and sexual violence. ACE-I Study – 2014 The ACE-I (Adverse Childhood Experiences International) study conducted in 2014 is a significant research endeavor that investigates the prevalence and impact of adverse childhood experiences on health and well-being across different countries. This study examines a range of adverse experiences such as abuse, neglect, household dysfunction, and other traumatic events, shedding light on their long-term effects on physical and mental health outcomes. The findings from the ACE-I study emphasize the critical importance of early intervention and prevention strategies to mitigate the negative consequences of childhood adversity and promote healthier outcomes for individuals and communities worldwide. WMHS – 2017 The data from the World Mental Health (WMH) survey provides a comprehensive understanding of social anxiety disorder (SAD) on a global scale. The study addresses the question of whether SAD is specific to Western cultures and reveals variations in prevalence and role impairment across different regions. The survey shows that SAD is a prevalent condition worldwide, typically emerging at an early age and persisting over time. It is associated with certain socio-demographic factors (such as younger age, female gender, unmarried status, lower education, and lower household income) and exhibits consistent comorbidity patterns with other mental health disorders. These findings underscore the clinical and public health significance of SAD on an international level. References 1. Adverse Childhood Experiences (ACEs). (1998). Centers for Disease Control and Prevention; U.S. Department of Health & Human Services Accessibility. https://www.cdc.gov/violenceprevention/aces/index.html 2. Bellis, M. A., Hughes, K., Leckenby, N., Perkins, C., & Lowey, H. (2014). National household survey of adverse childhood experiences and their relationship with resilience to health-harming behaviors in England. BMC Medicine, 1. https://doi.org/10.1186/1741-7015-12-72 3. Harvard Trauma Questionnaire. (1992). Harvard Program in Refugee Trauma; Harvard Program in Refugee Trauma. https://hprt-cambridge.org/screening/harvard-trauma-questionnaire 4. Kessler, R. C., & Walters, E. (1995). Textbook in Psychiatric Epidemiology (M. T. Tsuang & M. Tohen, Eds.; pp. 343–362). John Wiley & Sons, Inc. http://dx.doi.org/10.1002/0471234311 5. Kulka, R. A., Schlenger, W. E., Fairbank, J. A., Hough, R. L., Jordan, B. K., Marmar, C. R., & Weiss, D. S. (1988). National Vietnam Veterans Readjustment Study (NVVRS): Description, current status, and initial PTSD prevalence estimates. Washington, DC: Veterans Administration. 6. Stein, D. J., Lim, C. C. W., Roest, A. M., de Jonge, P., Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J., Benjet, C., Bromet, E. J., Bruffaerts, R., de Girolamo, G., Florescu, S., Gureje, O., Haro, J. M., Harris, M. G., He, Y., Hinkov, H., Horiguchi, I., Hu, C., … Scott, K. M. (2017). The cross-national epidemiology of social anxiety disorder: Data from the World Mental Health Survey Initiative. BMC Medicine, 1. https://doi.org/10.1186/s12916-017-0889-2 7. The National Intimate Partner and Sexual Violence Survey (NISVS) |Violence Prevention|Injury Center|CDC. (2011). Centers for Disease Control and Prevention; U.S. Department of Health & Human Services. https://www.cdc.gov/violenceprevention/datasources/nisvs/index.html
0 Comments
Trauma Series - Part 3 of 7
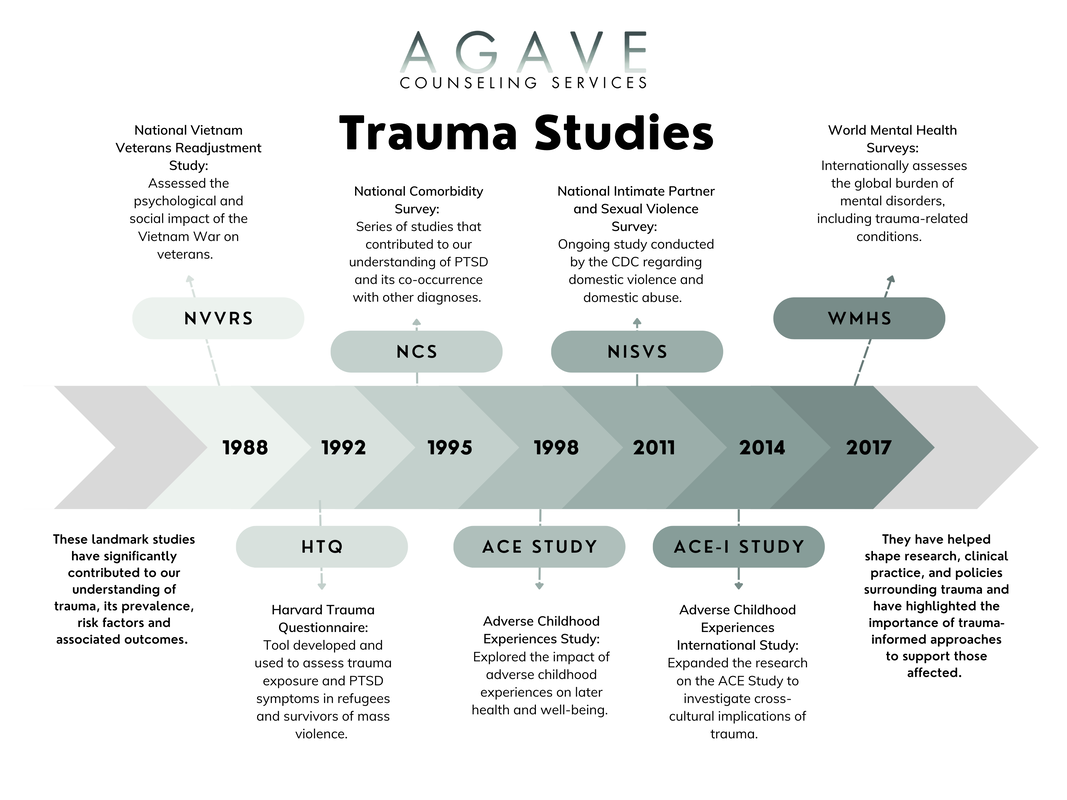
Experiencing trauma can have profound effects on an individual's mental, emotional, and physical well-being. It's important to recognize and understand the various symptoms associated with trauma to provide appropriate support and facilitate healing. In this blog post, we will delve into some common trauma symptoms to include addiction, avoidance, dissociation, flashbacks, hypervigilance, memory difficulties, mood swings, pain or illness, sleep problems, and suicidal ideation. By shedding light on these symptoms, we aim to promote awareness, empathy, and resilience in the face of trauma.
1. Addiction: Trauma can be a triggering factor for addiction, as individuals may turn to substances or behaviors to cope with emotional pain and distress (SAMHSA, 2014; ISTSS). Recognizing the link between trauma and addiction is crucial in seeking appropriate care. Engaging in therapy, support groups, and holistic approaches can aid in addressing underlying trauma while developing healthy coping mechanisms. 2. Avoidance: Avoidance is a common response to trauma, where individuals consciously or unconsciously try to steer clear of people, places, or situations that trigger distressing memories or emotions (APA, 2022). While avoidance may provide temporary relief, it can hinder the healing process long-term. Gradual exposure to triggers with the guidance of a therapist can empower individuals to reclaim control over their lives. 3. Dissociation: Dissociation is a defense mechanism that involves feeling disconnected from oneself, the environment, or the present moment (van der Kolk, 2014). It can manifest as a sense of detachment, amnesia, or feeling as though life is unreal (NIMH, 2023). Seeking therapy and engaging in grounding techniques can help individuals reconnect with their emotions, experiences, and regain a sense of stability. 4. Flashbacks: A flashback is the vivid and intrusive re-experiencing of a traumatic event, often making individuals feel as though they are reliving the trauma (APA, 2022). They can be triggered by sensory cues or emotional reminders. Coping strategies such as grounding techniques, deep breathing, and seeking professional support can help manage and process flashbacks effectively. 5. Hypervigilance: Hypervigilance refers to a heightened state of alertness and sensitivity to potential threats, often leading individuals to be constantly on guard (APA, 2022). This hypervigilance is a natural response to trauma, designed to protect against future harm. However, it can result in chronic anxiety and exhaustion. Practicing relaxation techniques, self-care, and seeking therapy can assist in managing hypervigilance and restoring a sense of safety. 6. Memory Difficulties: Trauma can impact memory processing, leading to difficulties with concentration, short-term memory, and recall (APA, 2022). These challenges can affect daily functioning and relationships. Strategies such as creating routines, using memory aids, and practicing mindfulness can help improve memory and cognitive function over time. 7. Mood Swings: Mood swings are common among individuals who have experienced trauma, with emotions fluctuating between extreme highs and lows (APA, 2022). These mood swings can be challenging to manage and may impact personal and professional relationships. Engaging in therapy, practicing self-care, and learning healthy emotion regulation techniques can aid in stabilizing mood fluctuations. 8. Pain or Illness: Physical symptoms such as chronic pain or unexplained illnesses can be associated with trauma (SAMHSA, 2014). Trauma can manifest in the body, leading to discomfort and distress. Integrating a holistic approach, which may include therapy, medication, relaxation techniques, and alternative therapies, can help alleviate physical symptoms and promote overall well-being. 9. Sleep Problems: Sleep disturbances, including insomnia, nightmares, and night terrors, are common among individuals who have experienced trauma (NIMH, 2023). Establishing a consistent sleep routine, practicing relaxation techniques before bed, and seeking therapy to address trauma-related sleep disturbances can help improve sleep quality and promote restorative rest. 10. Suicidal Ideation: Trauma can significantly impact an individual's mental health, leading to feelings of hopelessness and thoughts of self-harm or suicide (APA, 2022). It is crucial to take suicidal ideation seriously and seek immediate professional help. Therapeutic interventions, support systems, and safety planning can provide essential support for those experiencing such thoughts and promote resilience. In conclusion, trauma can leave deep imprints on individuals, affecting a multitude of aspects within their lives. By recognizing and understanding common trauma symptoms, such as the aforementioned, we can foster empathy and create a supportive environment for healing. Additionally, it is essential to seek professional help, build a strong support network, and practice self-care as part of the journey toward healing and recovery. References 1. American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787 2. Post-Traumatic Stress Disorder. (2023, May). National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd/index.shtml 3. Trauma-Informed Care in Behavioral Health Services. (2014). Substance Abuse and Mental Health Services Administration (SAMHSA). https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4816.pdf 4. Traumatic Stress and Substance Abuse Problems. (n.d.). International Society for Traumatic Stress Studies (ISTSS). Retrieved from https://istss.org/ISTSS_Main/media/Documents/ISTSS_TraumaStressandSubstanceAbuseProb_English_FNL.pdf 5. van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. Viking. Trauma Series - Part 2 of 7
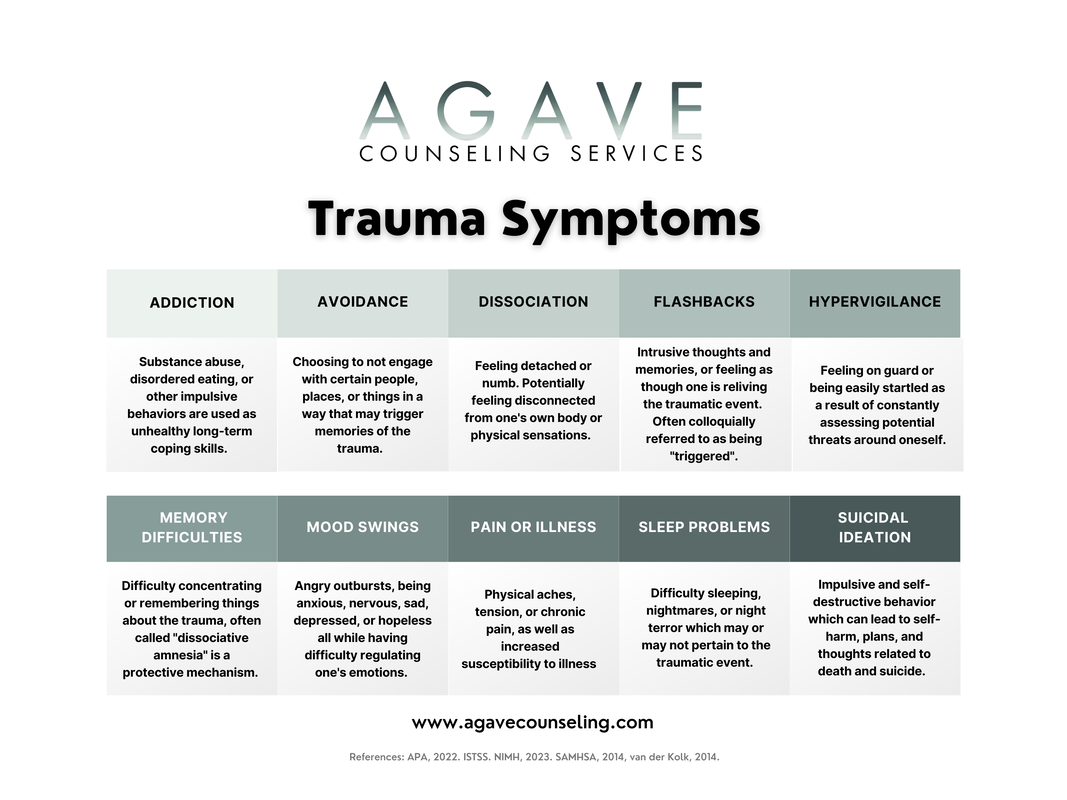
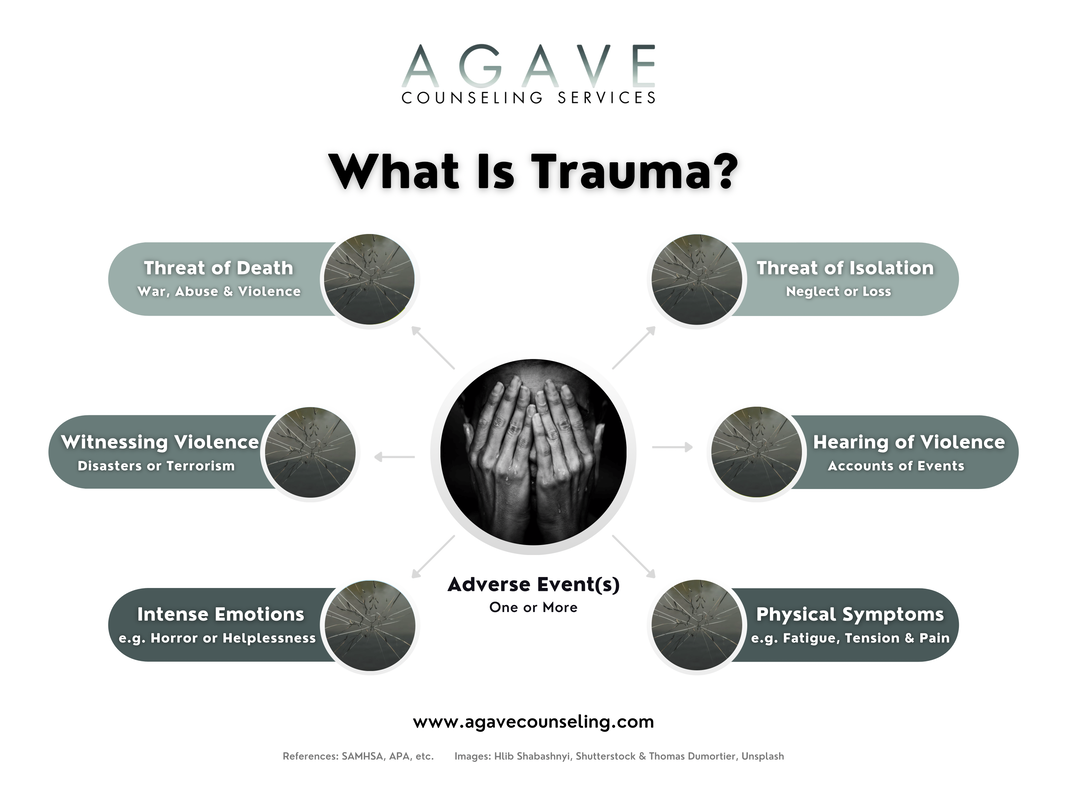
Trauma can be experienced in a number of different settings. Whether an event is deemed traumatic is defined by the 'subjective experience' of it rather than the event itself. Trauma often is categorized into four types.
TYPE 1 Often referred to as single-incident trauma which is sudden and unexpected, this trauma is limited in duration, and the individual experiences high levels of acute threat during the period of time in which the trauma occured. Examples could include severe illness, traumatic loss, an assault, witnessing violence, witnessing a disaster, combat incidents, childbirth, or other medical trauma. TYPE 2 Type two is referred to as complex trauma which can be trauma that was experienced by an individual as being long-lasting and ongoing over a period of time. Complex trauma can include experiences in childhood or early stages of development (even in utero), as well as experiences in adolescence and/or adulthood. Examples could include neglect, domestic violence, abuse, or the witnessing of neglect, domestic violence, or abuse. Additionally, bullying, coping with a chronic illness, or faith-based trauma. VICARIOUS TRAUMA Trauma does not only need to be experienced by an individual, for it to be distressing. Vicarious trauma can occur when the person who has experienced a trauma or witnessed a trauma firsthand communciates that trauma to another individual. The listener can experience trauma as well as similar, if not identical, symptoms that would be experienced by the person who had experienced the trauma. COLLECTIVE TRAUMA This trauma is characterized by psychological or emotional difficulties which can affect different communities, cultural groups, and generations. Adaptive and maladaptive coping patterns can be passed through communities intergenerationally, often referred to as "intergenerational trauma". Examples might include discrimination, sexism, racism, slavery, natural disasters, terrorism, experiences as a refugee, genocide, and or war. References 1. Friedman, M. J., Schnurr, P. P., & Keane, T. M. (2021). Handbook of PTSD, Third Edition. Guilford Publications. 2. Herman, Judith L. (2015). Trauma and recovery: The aftermath of violence from domestic abuse to political terror. Basic Books. 3. Herman, Judith Lewis. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 3, 377–391. https://doi.org/10.1002/jts.2490050305 4. McCann, I. L., & Pearlman, L. A. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 1, 131–149. https://doi.org/10.1007/bf00975140 Trauma Series - Part 1 of 7
Trauma can refer to any situation where a person experiences a significant amount of stress, fear, or danger, and feels that they are unable to cope with an event. Many people go through one or more experiences that they may consider to be distressing or traumatic events which can have an impact on their day-to-day functioning. Trauma can result in conscious and unconscious experiences that can plague our emotional, physical, and psychological well-being. Our understanding of trauma has expanded from the limited viewpoint that trauma can only be experienced by veterans and survivors of abuse, as well. It is also important to recognize that an event is subjectively deemed traumatic by the person experiencing the trauma, and should never be invalidated or attempted to be convinced otherwise.
Attending to trauma is crucial for mental health because traumatic experiences can have a profound impact on an individual's thoughts, emotions, and behaviors. Trauma can create persistent feelings of fear, anxiety, and depression, as well as negative beliefs about oneself and the world. These symptoms can lead to a range of mental health conditions, including post-traumatic stress disorder (PTSD), depression, and anxiety disorders. In some cases, trauma can also lead to physical health problems, such as chronic pain and autoimmune disorders. Furthermore, trauma is often interconnected with other social determinants of health, such as poverty, racism, and discrimination. Individuals who have experienced trauma may face additional barriers to accessing healthcare, education, and employment, which can further exacerbate mental health issues. Addressing trauma is therefore critical not only for individual mental health but also for social justice and equity. In recent years, there has been an increasing focus on trauma-informed care, which recognizes the impact of trauma and seeks to create safe, supportive environments for individuals who have experienced trauma. This approach emphasizes the importance of trust, safety, and empowerment in the healing process and promotes a collaborative, strengths-based approach to treatment. Trauma-informed care has been shown to be effective in reducing symptoms of trauma and improving mental health outcomes. In conclusion, the transformation of the word "trauma" to include adverse life experiences is an important development in our understanding of mental health. Addressing trauma is essential for promoting mental health and reducing health inequities. By recognizing the impact of trauma and promoting healing, we can work towards creating a more compassionate and resilient society. References 1. American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787 2. Bremner, J. D., & Marmar, C. R. (Eds.). (1998). Trauma, memory, and dissociation (pp. 242–250). American Psychiatric Press. 3. Der Kolk, B. V. (2015). The body keeps the score. Penguin Books. 4. Herman, J. L. (2015). Trauma and recovery: The aftermath of violence from domestic abuse to political terror. Basic Books. 5. Substance Abuse and Mental Health Services Administration. (2014). SAMHSA's Concept of Trauma and Guidance for a Trauma-Informed Approach. https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4884.pdf 6. World Health Organization. (2013). Guidelines for the management of conditions specifically related to stress. Geneva: World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/85119/9789241505406_eng.pdf In the creation of this website, there have been many creators who lent their work to support the design and overall theme of our page. In the history of business ownership, it is not uncommon for companies to fail to credit the creative time and work put forth by various artists and organizations that allow us to exist. This blog post is dedicated to the attribution of each image used within our site to each individual artist. Their hard work will not be taken advantage of and is wholeheartedly appreciated by Agave Counseling Services, LLC at large. Home PageHelena Lopes, Unsplash Erol Ahmed, Unsplash Billy Pasco, Unsplash www.icons8.com Mackenzie A. Cortese About PageWendy van Zyl, Pexels Amy Crooks Photography, LLC Casey Horner, Unsplash ServicesMitchell Lou, Unsplash Rates & FAQ'sErol Ahmed, Unsplash Contactwww.icons8.com Mackenzie A. Cortese Mackenzie A. Cortese Mackenzie A. Cortese
|
ExtrasFreebies & E-Courses ThemesRecent posts |












 RSS Feed
RSS Feed